How Gut Health Affects Mental Health: The Science of the Gut-Brain Axis
Have you ever felt “butterflies” in your stomach before a big presentation, or a “gut wrenching” sensation when receiving bad news? These aren’t just metaphors; they are physical manifestations of the complex communication network between your digestive system and For decades, the medical community treated the mind and the body as two separate entities. However, modern science has revealed a groundbreaking truth: your digestive system and your brain are in a constant, high-speed conversation. At Growing Minds Mental Health Services, we emphasize this connection because understanding how gut health affects mental health is essential for true, lasting healing.
In this comprehensive guide, we will explore the “Second Brain,” the role of the microbiome, and why your diet might be the missing piece in your mental health journey.
What is the Gut-Brain Axis?
To understand how gut health affects mental health, we must first look at the Gut-Brain Axis (GBA). This is a complex bidirectional communication network that includes the central nervous system (CNS) and the enteric nervous system (ENS).
The primary “highway” for this communication is the Vagus Nerve. This nerve runs from the brainstem all the way to the abdomen, sending constant updates about the state of your organs to your brain. When your gut is inflamed or imbalanced, it sends “distress signals” to the brain, which can manifest as psychological symptoms.
The Microbiome: Why Gut Health Affects Mental Health on a Cellular Level
Your gut is home to trillions of microorganisms, collectively known as the microbiome. These bacteria are not just “hitchhikers”; they are active participants in your chemical makeup.
1. Neurotransmitter Production
It is a common misconception that neurotransmitters are only produced in the brain. In reality, a significant portion of the chemicals that dictate your mood are manufactured in your gut:
- Serotonin: Approximately 95% of the body’s serotonin, the “feel-good” hormone, is produced in the gut.
- Dopamine: The chemical responsible for motivation and reward is also heavily influenced by gut bacteria.
- GABA: This amino acid helps control feelings of fear and anxiety; certain gut bacteria are primary producers of it.
2. The Role of Inflammation
When the lining of the gut becomes compromised—often called “leaky gut”—toxins can enter the bloodstream. This triggers an immune response and systemic inflammation. Research shows that chronic inflammation is a primary driver for clinical depression and anxiety disorders. This is a key reason why gut health affects mental health so directly; an inflamed gut often leads to an inflamed brain.
Clinical Evidence: How Poor Gut Health Affects Mental Health Disorders
The link between the gut and the mind is more than just a theory; it is backed by rigorous clinical studies.
- Anxiety and Stress: Studies have shown that patients with various digestive disorders, such as Irritable Bowel Syndrome (IBS), have significantly higher rates of co-occurring anxiety.
- Depression: Research published in Nature Microbiology identified specific gut bacteria that are consistently missing in people with depression, suggesting that replacing these microbes could improve depressive symptoms.
- Cognitive Function: Ever experienced “brain fog”? This is often a result of gut dysbiosis affecting the brain’s ability to process information clearly.
| Factor | Impact on Gut Health | Resulting Mental State |
| Processed Sugar | Feeds harmful bacteria | Increased irritability and “sugar crashes” |
| Probiotics | Increases microbial diversity | Improved emotional regulation |
| Chronic Stress | Weakens gut lining | Heightened cortisol and anxiety |
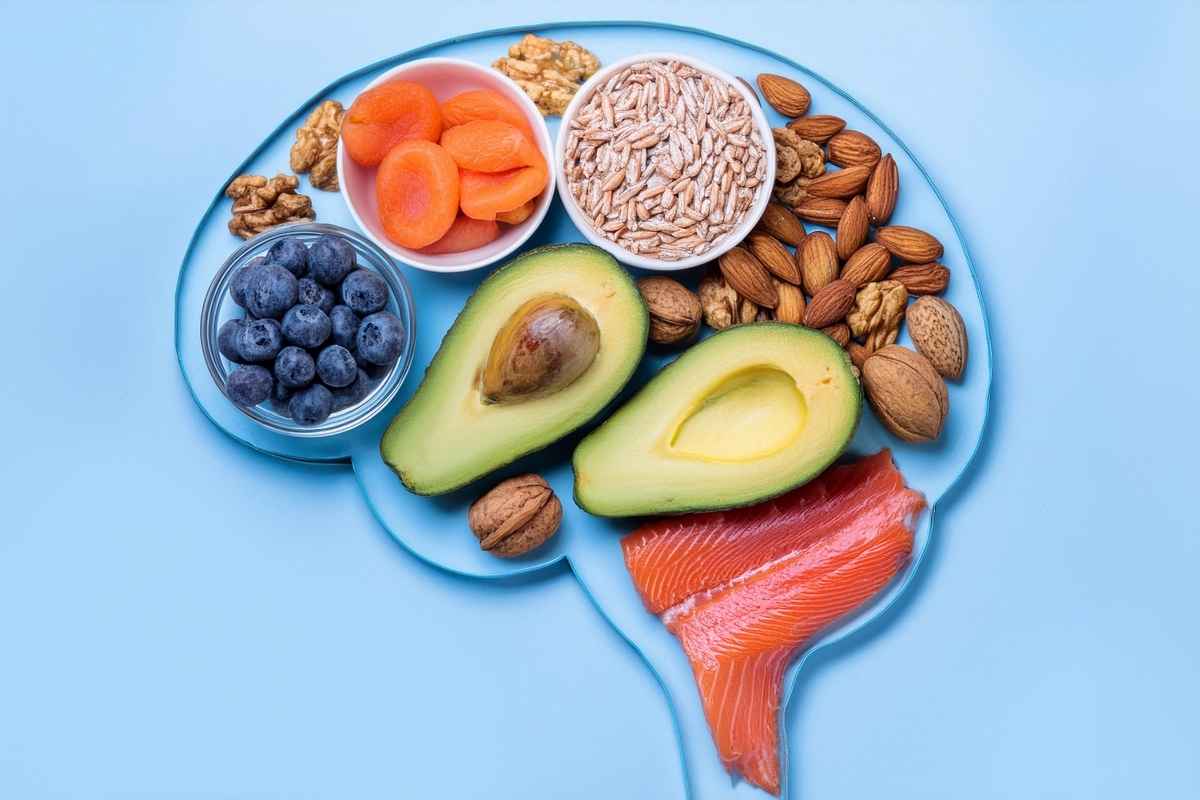
Actionable Steps: Improving How Your Gut Health Affects Mental Health
Knowing that gut health affects mental health gives you a powerful tool for recovery. You can begin to influence your mental state through your plate:
- Prioritize Fermented Foods: Incorporate kefir, sauerkraut, kimchi, and kombucha to introduce beneficial live cultures.
- Increase Prebiotic Fiber: Feed your “good” bacteria with garlic, onions, leeks, and asparagus.
- Limit Ultra-Processed Foods: High-sugar and highly processed foods can kill off beneficial microbes, leading to mood instability.
- Manage Stress: Since the communication is bidirectional, high stress can actually damage your gut bacteria, creating a vicious cycle.
Holistic Support at Growing Minds Mental Health Services
Understanding the biological roots of your emotions is empowering, but you don’t have to navigate this journey alone. Because we know how deeply gut health affects mental health, our therapeutic approach considers the whole person—mind, body, and lifestyle.
If you feel like you’ve been struggling with your mood despite trying traditional methods, it may be time to look at the deeper connection between your gut and your mind.
Take the first step toward comprehensive well-being today.
Contact Growing Minds Mental Health Services to schedule a consultation and discover how a holistic approach can transform your mental health.
Below are links to some clinical evidences that proves link between gut health and mental health:
Foundational Studies:
- Valles-Colomer, M., et al. (2019). “The neuroactive potential of the human gut microbiota in quality of life and depression.” Nature Microbiology. View on PubMed
- Cryan, J. F., & Dinan, T. G. (2012). “Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour.” Nature Reviews Neuroscience. View on Nature
- Foster, J. A., & Neufeld, K. M. (2013). “Gut–brain axis: how the microbiome influences anxiety and depression.” Trends in Neurosciences. View on Cell/Trends
- Kelly, J. R., et al. (2016). “Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat.” Journal of Psychiatric Research. View on PubMed
- Mayer, E. A., et al. (2015). “Gut/brain axis and the microbiota.” The Journal of Clinical Investigation. View on JCI
- Strandwitz, P., et al. (2019). “GABA-modulating bacteria of the human gut microbiota.” Nature Microbiology. View on Nature
- Slykerman, R. F., et al. (2017). “Effect of Lactobacillus rhamnosus HN001 in Pregnancy on Postpartum Symptoms of Depression and Anxiety.” EBioMedicine. View on Lancet/EBioMedicine
- Rao, S. C., et al. (2018). “Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis.” Clinical and Translational Gastroenterology. View on PMC
Recent studies:
- Kamath, S., et al. (2025). “Distinguishing the causative, correlative and bidirectional roles of the gut microbiota in mental health.” Nature Mental Health. This landmark study utilizes advanced modeling to separate whether gut changes cause mental illness or simply mirror it, providing the strongest evidence to date for a causal link in depression and schizophrenia. View Study on Nature
- Duke-NUS Medical School (2025). “Scientists reveal gut microbes’ hidden role in anxiety.” ScienceDaily. This February 2025 report details how specific microbial metabolites, called indoles, act like a “clutch” in the brain to prevent neurons in the amygdala from over-firing, directly reducing anxiety behaviors. View Article on ScienceDaily
- Schachter, J., et al. (2024). “How mental states impact gut health.” Max-Planck-Gesellschaft. Published in late 2024, this research identified a direct circuit from the brain’s amygdala (the fear center) to the Brunner’s glands in the gut, proving that stress directly suppresses beneficial Lactobacilli bacteria. View Research Summary
- Toader, et al. (2024). “Mind, Mood and Microbiota—Gut–Brain Axis in Psychiatric Disorders.” MDPI. A 2024 comprehensive review focusing on “psychobiotics” (probiotics for the mind), demonstrating how multi-strain formulations can increase the Firmicutes-to-Bacteroidetes ratio to alleviate symptoms of Major Depressive Disorder (MDD). View Full Text on MDPI
- Frontiers in Microbiology (2024). “Depression-associated gut microbes, metabolites and clinical trials.” This review catalogs the latest clinical trials involving Lactobacillus acidophilus and Bifidobacterium longum, showing their efficacy in modulating the 5-HT (serotonin) pathway to treat depression. View Study on Frontiers
- Cureus (2025). “The Gut-Brain Axis and Mental Health: How Diet Shapes Our Cognitive and Emotional Well-Being.” A 2025 update that underscores the role of Short-Chain Fatty Acids (SCFAs) as the primary chemical messengers that cross the blood-brain barrier to regulate neuroinflammation. View on PubMed Central
- Mayo Clinic (Ongoing 2024-2025). “Microbiome of Depression & Treatment Response to Citalopram.” This active clinical trial is investigating how the gut microbiome changes in response to standard antidepressants, aiming to use gut bacteria as a biomarker to predict which patients will respond to therapy. View Trial Details on ClinicalTrials.gov